Healthcare has always been reactive – we treat diseases after symptoms appear. But what if we could predict and prevent illnesses before they manifest?
This isn’t science fiction anymore. The integration of Artificial Intelligence (AI) with wearable technology is fundamentally transforming healthcare from a reactive to a proactive model, creating unprecedented opportunities for early intervention and robust disease prevention.
The shift is undeniable. The global wearable medical devices market is experiencing exponential growth, projected to reach $195 billion by 2027. However, beyond market figures lies a more compelling story: wearables powered by AI are saving lives by detecting health anomalies years before traditional diagnostics would have caught them. From identifying irregular heart rhythms that could lead to stroke, to monitoring glucose levels that prevent diabetic complications, these devices represent a paradigm shift in how we approach health management.
For healthcare organizations, medical device manufacturers, and digital health startups, understanding this transformation isn’t optional – it’s imperative.
In this detailed article, we will explore the technical architecture, the crucial clinical applications, the compelling business implications, and the specific implementation strategies for deploying AI-powered preventive healthcare through wearables.
- The Architecture of AI-Powered Wearable Health Systems
- Clinical Applications: How Wearables Prevent Diseases
- Business Case: ROI and Economic Impact
- Emerging AI Features and Next-Generation Wearable Devices
- Technical Foundations for AI-Driven Healthcare Wearables
- How Developex Supports AI-Driven Healthcare Wearables
- Final Thoughts
The Architecture of AI-Powered Wearable Health Systems
AI-powered wearable health systems rely on a connected architecture that links sensors, devices, and cloud intelligence into one cohesive ecosystem. This structure enables seamless data flow, real-time insights, and adaptive personalization for users. Understanding the architecture helps product teams identify where innovation, scalability, and differentiation can be achieved within the health technology value chain.
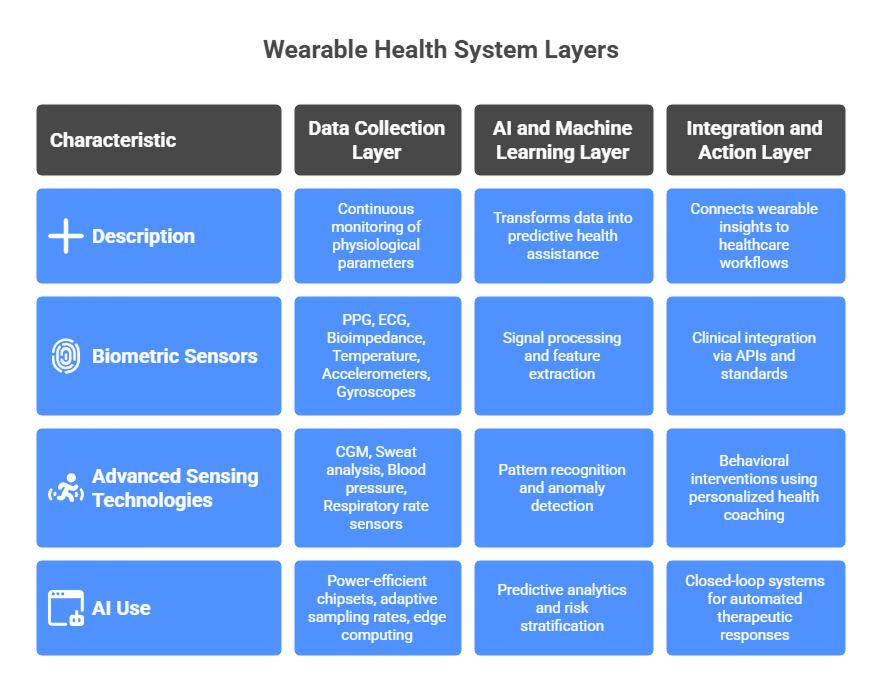
Data Collection Layer: Beyond Simple Tracking
Modern health wearables have evolved far beyond basic step counting. Today’s devices incorporate sophisticated sensor arrays that continuously monitor multiple physiological parameters:
Biometric Sensors:
- Photoplethysmography (PPG) sensors measure heart rate, heart rate variability (HRV), blood oxygen saturation (SpO2), and can even estimate blood pressure through pulse wave analysis
- Electrocardiogram (ECG) sensors capture electrical heart activity, enabling detection of arrhythmias like atrial fibrillation
- Bioimpedance sensors measure body composition, hydration levels, and can detect fluid retention – critical for heart failure management
- Temperature sensors track baseline body temperature and detect deviations that may indicate infection or metabolic changes
- Accelerometers and gyroscopes monitor movement patterns, sleep quality, gait analysis, and fall detection
Advanced Sensing Technologies:
- Continuous glucose monitors (CGMs) using subcutaneous sensors provide real-time glucose data every 5-15 minutes
- Sweat analysis sensors detect electrolyte levels, cortisol, and lactate – valuable for hydration status and stress monitoring
- Blood pressure sensors using oscillometric or photoplethysmographic methods enable continuous or on-demand readings
- Respiratory rate sensors track breathing patterns during sleep and activity
The technical challenge isn’t just collecting this data – it’s doing so continuously, accurately, and with minimal battery consumption. Modern wearables achieve this through power-efficient chipsets, adaptive sampling rates that increase frequency when anomalies are detected, and edge computing that processes data locally before transmission.
AI and Machine Learning Layer: Turning Data into Insights
Raw sensor data is meaningless without intelligent interpretation. This is where AI transforms wearables from data collectors into predictive health assistants. The AI architecture typically includes:
Signal Processing and Feature Extraction: Machine learning algorithms first clean and process raw sensor signals, removing noise and artifacts caused by movement or environmental factors. Advanced digital signal processing techniques extract meaningful features: HRV metrics from ECG data, sleep stages from movement and heart rate patterns, stress indicators from autonomic nervous system activity.
Pattern Recognition and Anomaly Detection: Deep learning models, particularly convolutional neural networks (CNNs) and recurrent neural networks (RNNs), excel at identifying patterns in time-series physiological data. These models learn individual baselines for each user – understanding what’s “normal” for that specific person – then flag deviations that may indicate health issues.
For example, an LSTM (Long Short-Term Memory) neural network can analyze weeks of heart rate data to establish a user’s typical circadian rhythm, exercise response, and stress patterns. When the model detects sustained deviations – perhaps elevated resting heart rate combined with reduced HRV – it can predict potential illness days before symptoms appear.
Predictive Analytics and Risk Stratification: The most sophisticated wearable AI systems don’t just detect current problems – they predict future risks. By combining wearable data with electronic health records, genetic information, and population health data, machine learning models can calculate individualized risk scores for various conditions.
Gradient boosting algorithms and ensemble methods integrate multiple data sources to predict outcomes like:
- Likelihood of developing type 2 diabetes within 5 years based on glucose variability patterns
- Risk of cardiovascular events using HRV, blood pressure trends, and activity levels
- Probability of hospital readmission for heart failure patients based on weight, fluid retention, and activity changes
- Sleep apnea risk from nocturnal oxygen desaturation and breathing pattern analysis
Personalization and Adaptive Learning: Modern wearable AI systems employ reinforcement learning to continuously improve their accuracy for individual users. The system learns which interventions work best for each person, optimizing recommendations over time. If activity reminders at 2 PM consistently increase a user’s daily steps, the system reinforces this timing. If stress reduction prompts during meetings are ignored, it adapts the timing and format.
Integration and Action Layer: Closing the Loop
Data collection and analysis are valuable only if they drive meaningful action. The integration layer connects wearable insights to healthcare workflows and user behaviors:
Clinical Integration: APIs and interoperability standards (FHIR, HL7) enable wearable data to flow into electronic health records, giving clinicians comprehensive longitudinal data. Remote patient monitoring platforms aggregate wearable data from multiple devices, applying clinical decision support algorithms to prioritize patients needing intervention.
Behavioral Interventions: Just-in-time adaptive interventions (JITAIs) use AI to deliver personalized health coaching at optimal moments. Natural language processing powers conversational interfaces that provide contextually relevant guidance: “Your stress levels have been elevated for 3 hours. Would you like to try a 5-minute breathing exercise?”
Closed-Loop Systems: The ultimate integration: automated therapeutic responses. Insulin pumps that adjust delivery based on CGM readings. Cardiac pacemakers that modify pacing based on activity levels. Vagus nerve stimulators that detect seizure onset from wearable EEG and deliver preventive stimulation.
Clinical Applications: How Wearables Prevent Diseases
AI-driven clinical applications in wearables are moving beyond fitness tracking toward active disease prevention and early diagnostics. By continuously monitoring biomarkers and detecting subtle deviations, these systems enable timely interventions, reduce healthcare costs, and support a shift from reactive to preventive care.
Diabetes Prevention and Management: Continuous Intelligence
Diabetes affects 537 million adults globally, with another 541 million at high risk (prediabetes). The disease’s complications – blindness, kidney failure, amputations, heart disease – result primarily from poor glucose control. Wearables are transforming diabetes care:
Continuous Glucose Monitoring (CGM) and AI Analytics: CGM devices measure interstitial glucose every 5-15 minutes, generating 288 data points daily – compared to 4-6 fingerstick tests with traditional monitoring. But raw glucose data overwhelms users and clinicians. AI makes it actionable.
Machine learning algorithms analyze CGM data to identify patterns:
- Postprandial glucose responses to different foods, revealing personal glycemic index variations
- Dawn phenomenon patterns indicating when basal insulin needs adjustment
- Exercise-induced hypoglycemia risk, enabling preventive carbohydrate intake
- Medication efficacy windows, optimizing timing for maximum benefit
Predictive Glucose Monitoring: Advanced AI models predict glucose levels 30-60 minutes in advance with 95% accuracy. These predictions enable preemptive interventions: consuming fast-acting carbohydrates before predicted hypoglycemia, administering correction insulin before predicted hyperglycemia, adjusting exercise intensity based on glucose trajectory.
The clinical impact is measurable: studies show AI-guided CGM use increases time in optimal glucose range from 50% to 75%, reducing HbA1c by 1-2% and cutting hypoglycemic events by 60%. These improvements translate directly to reduced complications: every 1% HbA1c reduction decreases microvascular complication risk by 37%.
Prediabetes Detection and Intervention: Even more promising is wearables’ role in preventing diabetes development. AI algorithms analyzing CGM data from individuals without diabetes can detect subtle glucose dysregulation – impaired fasting glucose, elevated postprandial responses, reduced glucose variability – that predict type 2 diabetes years before diagnosis.
Combined with activity tracking and weight monitoring, these insights enable targeted lifestyle interventions during the reversible prediabetes phase. Research indicates that preventing progression from prediabetes to diabetes in just 10% of high-risk individuals would save $3.7 billion annually in the United States alone.
Cardiovascular Disease Prevention: The Biggest Impact
Cardiovascular disease remains the leading cause of death globally, claiming 17.9 million lives annually. AI-powered wearables are making significant inroads in prevention:
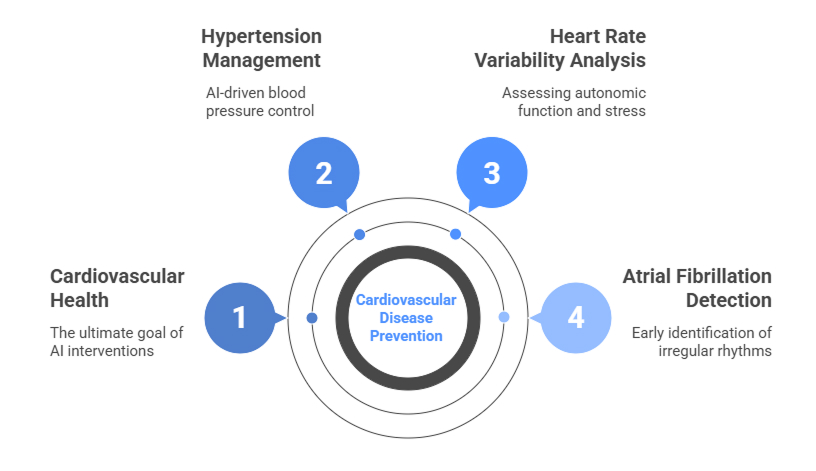
Atrial Fibrillation Detection: Wearables enable large-scale, population-level screening, successfully identifying irregular heart rhythms, as demonstrated by the Apple Heart Study (over 400,000 participants). Because Atrial Fibrillation (AFib) is often subclinical and intermittent, continuous monitoring is critical for early detection. Catching these episodes allows for the timely initiation of anticoagulation therapy, which is proven to reduce stroke risk by up to 70% in high-risk patients. Furthermore, AI-guided personalized anticoagulation is an active area of research to optimize therapy and minimize bleeding risks.
Heart Rate Variability and Autonomic Function: HRV – the variation in time intervals between heartbeats – provides a window into autonomic nervous system health. Low HRV indicates poor cardiovascular health and predicts mortality risk. AI algorithms analyze HRV patterns across different contexts (sleep, rest, exercise recovery) to assess cardiovascular fitness and stress load.
Research shows that sustained low HRV precedes heart attacks by days or weeks. Wearables that track HRV trends can trigger preventive interventions: medication adjustments, stress reduction programs, or urgent clinical evaluation.
Blood Pressure Monitoring and Hypertension Management: Hypertension affects 1.3 billion people but remains poorly controlled in most patients. Traditional blood pressure monitoring – occasional clinic readings or periodic home measurements – misses the dynamic patterns that drive cardiovascular damage.
Continuous blood pressure monitoring through wearables reveals patterns invisible to traditional methods: morning surges associated with stroke risk, nocturnal non-dipping linked to kidney damage, stress-induced spikes during work hours. AI analyzes these patterns alongside activity, sleep, and medication adherence data to optimize treatment strategies.
A study in the European Heart Journal found that AI-guided hypertension management using wearable data achieved blood pressure control in 87% of patients, compared to 57% with standard care – a 53% relative improvement.
Sleep Disorders and Mental Health: The Hidden Epidemic
Sleep disorders affect over 50 million Americans, with 80% of cases undiagnosed. Poor sleep drives numerous health problems: obesity, diabetes, cardiovascular disease, cognitive decline, depression. Wearables are making sleep health visible and actionable:
Sleep Apnea Screening: Obstructive sleep apnea (OSA) affects 1 billion people globally, with 85% of moderate-to-severe cases undiagnosed. OSA causes repeated breathing cessations during sleep, reducing oxygen levels and fragmenting sleep. Long-term consequences include hypertension, heart disease, and stroke.
Wearable devices using pulse oximetry, respiratory rate detection, and movement analysis can screen for sleep apnea with 85-90% accuracy compared to polysomnography. AI algorithms identify characteristic patterns: repetitive oxygen desaturations, increased heart rate variability during desaturations, and interrupted breathing.
Early screening enables prompt diagnosis and treatment with CPAP therapy, which reduces cardiovascular event risk by 40% and improves quality of life significantly.
Sleep Quality Optimization: Beyond disorder detection, wearables optimize sleep quality through AI-powered insights:
- Identifying optimal bedtimes based on circadian rhythm analysis
- Detecting environmental factors affecting sleep (temperature, noise, light)
- Analyzing sleep stage transitions to determine ideal wake times
- Correlating daytime behaviors (caffeine, exercise, screen time) with sleep quality
Mental Health Monitoring: Depression and anxiety affect 280 million and 301 million people globally, respectively. These conditions often develop gradually, with objective signs preceding subjective awareness.
Wearables detect mental health changes through passive monitoring:
- Reduced physical activity and social interaction (via location and Bluetooth proximity data)
- Disrupted sleep patterns and circadian rhythm irregularities
- Elevated resting heart rate and reduced HRV indicating chronic stress
- Changes in speech patterns captured by smartphone microphones (with consent)
AI models trained on these digital biomarkers can predict depressive episodes days to weeks in advance with 80-85% accuracy. Early detection enables timely intervention – therapy adjustments, increased clinical contact, social support mobilization – preventing crisis situations.
Cancer Prevention: Early Detection Through Biosignals
While wearables can’t prevent cancer’s initial cellular mutations, they’re showing promise in early detection, when treatment is most effective:
Baseline Deviation Detection: Many cancers cause subtle physiological changes long before clinical symptoms appear. AI algorithms that establish individual baselines can detect these deviations:
- Persistent resting heart rate elevation (indicating systemic inflammation)
- Unexplained weight loss patterns
- Chronic sleep disruption
- Sustained low HRV suggesting autonomic dysfunction
- Elevated resting metabolic rate
While none of these signs are cancer-specific, unusual combinations flagged by AI can prompt timely screening. Studies show that algorithm-flagged individuals had 3-4 times higher cancer detection rates compared to routine screening protocols.
Post-Treatment Monitoring: For cancer survivors, wearables enable continuous surveillance for recurrence signs: activity decline, weight changes, sleep disruption. AI models trained on patient-specific recovery trajectories can detect deviations indicating possible recurrence months earlier than scheduled imaging.
Infectious Disease: Outbreak Detection and Management
The COVID-19 pandemic highlighted wearables’ potential in infectious disease management:
Early Symptom Detection: Multiple studies demonstrated that wearable-detected changes – elevated resting heart rate, reduced HRV, increased respiratory rate, elevated skin temperature – preceded COVID-19 symptoms by 1-3 days. AI models analyzing these patterns achieved 80% accuracy in predicting infection before symptom onset.
Early detection enables immediate isolation, reducing transmission. At population scale, aggregated wearable data provides early outbreak warnings, enabling public health responses before traditional surveillance detects increases.
Disease Progression Monitoring: For infected individuals, continuous monitoring tracks disease severity: persistent oxygen desaturation indicating potential hospitalization need, respiratory rate trends suggesting pneumonia development. This enables home-based care with safety monitoring, reducing healthcare system burden.
| Clinical Area | Key Biomarkers / Data | AI Function | Preventive Outcome |
| Cardiovascular Health | ECG, HRV, BP, SpO₂, activity | Arrhythmia detection, HRV trend analysis, BP pattern modeling | Early AFib detection, hypertension management, stress monitoring |
| Diabetes Management | Continuous glucose data, activity, meals | Predictive glucose modeling, pattern recognition | Prevents hypo/hyperglycemia; supports lifestyle adjustments |
| Prediabetes Detection | Glucose variability, fasting patterns | Subclinical glucose dysregulation detection | Identifies prediabetes early; enables diet and exercise interventions |
| Sleep & Mental Health | Sleep stages, HRV, SpO₂, activity, speech, circadian data | Sleep apnea detection, mood prediction, circadian optimization | Early intervention for OSA, depression, anxiety; improved recovery |
| Cancer Monitoring | HR, HRV, metabolism, weight, sleep | Baseline deviation analysis, recurrence tracking | Early screening triggers, relapse detection |
| Infectious Disease | HR, HRV, temperature, SpO₂, respiration | Early infection prediction, outbreak modeling | Identifies infection before symptoms; supports outbreak response |
Business Case: ROI and Economic Impact
AI-driven wearables are shifting healthcare from reactive care to predictive efficiency. Their business value lies in measurable returns – from cost savings and resource optimization to new revenue models built on continuous data insights.
Healthcare Cost Reduction
The financial argument for AI-powered wearables is compelling:
Reduced Hospital Admissions: Remote patient monitoring with wearables reduces hospital readmissions by 25-40% for chronic disease patients. For heart failure alone – where 30-day readmission rates exceed 20% – this translates to massive savings. At $13,000 per hospitalization and 1 million heart failure admissions annually in the U.S., a 30% reduction saves $3.9 billion yearly.
Emergency Department Diversion: Early intervention triggered by wearable alerts prevents emergency situations requiring ED visits. Studies show 15-25% ED visit reductions for monitored patients. With average ED costs of $1,400 and 145 million annual visits, even modest reductions yield substantial savings.
Complication Prevention: The true ROI comes from preventing disease progression and complications:
- Preventing diabetes in high-risk individuals saves $13,700 per person over 10 years
- Preventing stroke through AFib detection saves $100,000-230,000 per event
- Preventing heart failure hospitalization saves $23,000-40,000 per admission
- Preventing diabetic foot ulcers saves $20,000-50,000 per ulcer (and potential amputation costs exceeding $100,000)
Productivity Gains: Beyond healthcare costs, disease prevention generates economic value through maintained workforce productivity. Chronic diseases cause 130 million lost workdays annually in the U.S., costing $260 billion in lost productivity. Preventing disease progression maintains worker productivity and quality of life.
Revenue Models for Healthcare Organizations
Remote Patient Monitoring Reimbursement: Medicare and most insurers now reimburse remote patient monitoring services. CPT codes 99453, 99454, 99457, and 99458 cover device setup, data collection, and clinical interpretation, generating $100-150 per patient monthly. For a healthcare system monitoring 10,000 chronic disease patients, this represents $12-18 million annual revenue.
Value-Based Care Performance: Under value-based payment models, healthcare organizations earn bonuses for quality metrics and cost savings. Wearable-enabled preventive care improves multiple quality measures:
- Diabetes control (HbA1c <8%)
- Blood pressure control (<140/90)
- Medication adherence rates
- Preventive service completion
- Patient satisfaction scores
Organizations achieving these metrics earn 3-7% bonuses on total patient care costs – tens of millions for large systems.
Employer Wellness Programs: Employers spend $3.7 trillion annually on employee health benefits. Wearable-based wellness programs reduce costs through:
- Lower health insurance premiums (2-5% reduction)
- Reduced absenteeism (28% reduction in sick days)
- Improved presenteeism (20% productivity increase)
- Lower workers’ compensation claims
Large employers invest $300-500 per employee in wellness programs, creating a $12-20 billion market. Effective wearable programs demonstrate 3:1 ROI within 2-3 years.
Emerging AI Features and Next-Generation Wearable Devices
The future of preventive healthcare wearables lies in next-generation devices that combine advanced sensors with AI-driven capabilities. These innovations are transforming how we monitor health, predict disease, and deliver personalized care.
Advanced Biosensors on the Horizon
Emerging wearables are integrating non-invasive biosensors to measure biomarkers that were previously difficult to track outside a clinical setting. Examples include:
- Non-invasive glucose and cholesterol monitoring.
- Continuous cuffless blood pressure monitoring.
- Multi-biomarker smart patches measuring hydration, stress hormones, lactate, and inflammation.
These innovations rely on embedded systems and low-power firmware capable of accurate, real-time data capture.
AI Features Transforming Preventive Care
AI continues to expand the capabilities of wearables:
- Digital biomarkers: Early detection of neurodegenerative diseases like Parkinson’s or Alzheimer’s through gait, voice, or motor pattern analysis.
- Context-aware behavioral nudges: Personalized recommendations for diet, exercise, sleep, and medication adherence.
- Predictive health scoring: Risk stratification to identify users who may need early medical intervention.
- Generative AI companions: Conversational coaching and support integrated directly into apps for user engagement and adherence.
Ecosystem Integration
Next-generation wearables are increasingly connected to the broader healthcare ecosystem:
- Telemedicine and EHR integration for remote monitoring and clinician oversight.
- Predictive dashboards for caregivers and healthcare professionals.
- Population-level AI models optimized for different age groups, lifestyles, and chronic conditions.
Technical Foundations for AI-Driven Healthcare Wearables
Developing AI-powered preventive healthcare wearables requires a careful balance of hardware design, embedded software, AI integration, and regulatory compliance. Understanding these technical foundations is essential for creating reliable, accurate, and user-friendly devices.
Embedded Development Challenges
Wearables rely on embedded systems to continuously collect, process, and transmit health data. Key challenges include:
- Multi-sensor integration: Combining ECG, PPG, SpO₂, accelerometers, and glucose sensors into a single device.
- Low-power firmware: Ensuring devices can operate 24/7 without frequent charging.
- Edge AI vs Cloud AI: Deciding whether AI inference occurs on-device (for real-time response) or in the cloud (for complex predictive analytics).
- Latency and reliability: Processing critical health data with minimal delay to enable timely alerts.
Software Development Specifications
The companion software ecosystem is just as critical as the device itself. Specifications include:
- Secure data transmission: Bluetooth LE, Wi-Fi, and NFC protocols with encryption.
- Cross-platform companion apps: iOS and Android apps for visualization, alerts, and integration with telemedicine platforms.
- Data pipelines for AI/ML models: Efficient storage, training, and deployment of predictive algorithms.
- OTA (Over-the-Air) updates: For firmware and AI models to ensure devices stay current with new features and accuracy improvements.
- User experience and accessibility: Intuitive interfaces that support adherence and engagement.
Compliance and Security
Healthcare wearables must adhere to strict regulations to protect patient data and ensure device reliability:
- HIPAA/GDPR compliance for secure handling of personal health information.
- Data encryption and anonymization across storage and transmission.
- Accuracy validation and certification readiness for medical-grade devices.
By mastering these technical foundations, companies can create wearables that not only capture health data but also transform it into actionable AI-driven insights, supporting preventive healthcare at scale.
How Developex Supports AI-Driven Healthcare Wearables
Creating reliable, AI-powered preventive healthcare wearables requires expertise across embedded development, software engineering, AI integration, and regulatory compliance. Developex helps innovators bring these complex devices to market efficiently, safely, and effectively.
Embedded Development Expertise: Developex designs embedded systems capable of integrating multiple sensors, including ECG, PPG, SpO₂, and glucose monitors. Our engineers optimize low-power firmware for continuous operation, enabling wearables to function 24/7 without compromising accuracy. We also implement edge AI, allowing real-time analysis directly on the device.
Companion App Development: Our team develops cross-platform companion apps for iOS and Android, providing users and clinicians with intuitive data visualization, alerts, and health insights. These apps integrate seamlessly with telemedicine platforms, supporting remote patient monitoring and proactive health management.
AI/ML Integration: Developex implements AI and ML algorithms to turn raw health data into actionable insights. From predictive analytics for chronic disease management to personalized recommendations for sleep, activity, and stress, our solutions enable preventive healthcare wearables to deliver measurable outcomes.
QA and Security: We ensure that devices meet medical-grade reliability standards and comply with HIPAA, GDPR, and other regulations. Our QA processes cover accuracy testing, secure data transmission, and OTA updates for both firmware and AI models, guaranteeing safety, security, and user trust.
Flexible Engagement Models: Developex offers tailored collaboration models:
- End-to-end development: From concept and prototyping to full deployment.
- Team augmentation: Extending in-house teams with specialized embedded and AI expertise.
By combining deep technical knowledge with healthcare domain experience, Developex helps companies deliver AI-powered wearables that are reliable, secure, and capable of transforming preventive healthcare.
Final Thoughts
The rise of AI-powered preventive healthcare wearables is transforming the way we approach health and wellness. By continuously monitoring vital signs, analyzing data with predictive analytics, and delivering personalized recommendations, these devices shift healthcare from reactive treatment to proactive, preventive care.
From smartwatches and fitness trackers to continuous glucose monitors, biosensor patches, and medical-grade wearables, the combination of embedded systems, AI integration, and companion apps is enabling earlier interventions, improved chronic disease management, and better overall health outcomes.
For innovators and medical providers, partnering with an experienced healthcare software development provider like Developex ensures that wearables are not only technologically advanced but also secure, reliable, and compliant. With expertise in embedded software, AI/ML integration, QA, and cross-platform app development, Developex bridges the gap between concept and market-ready devices, empowering the next generation of preventive healthcare solutions.
The future of healthcare is proactive, data-driven, and wearable — and with the right technology partner, it’s within reach today.